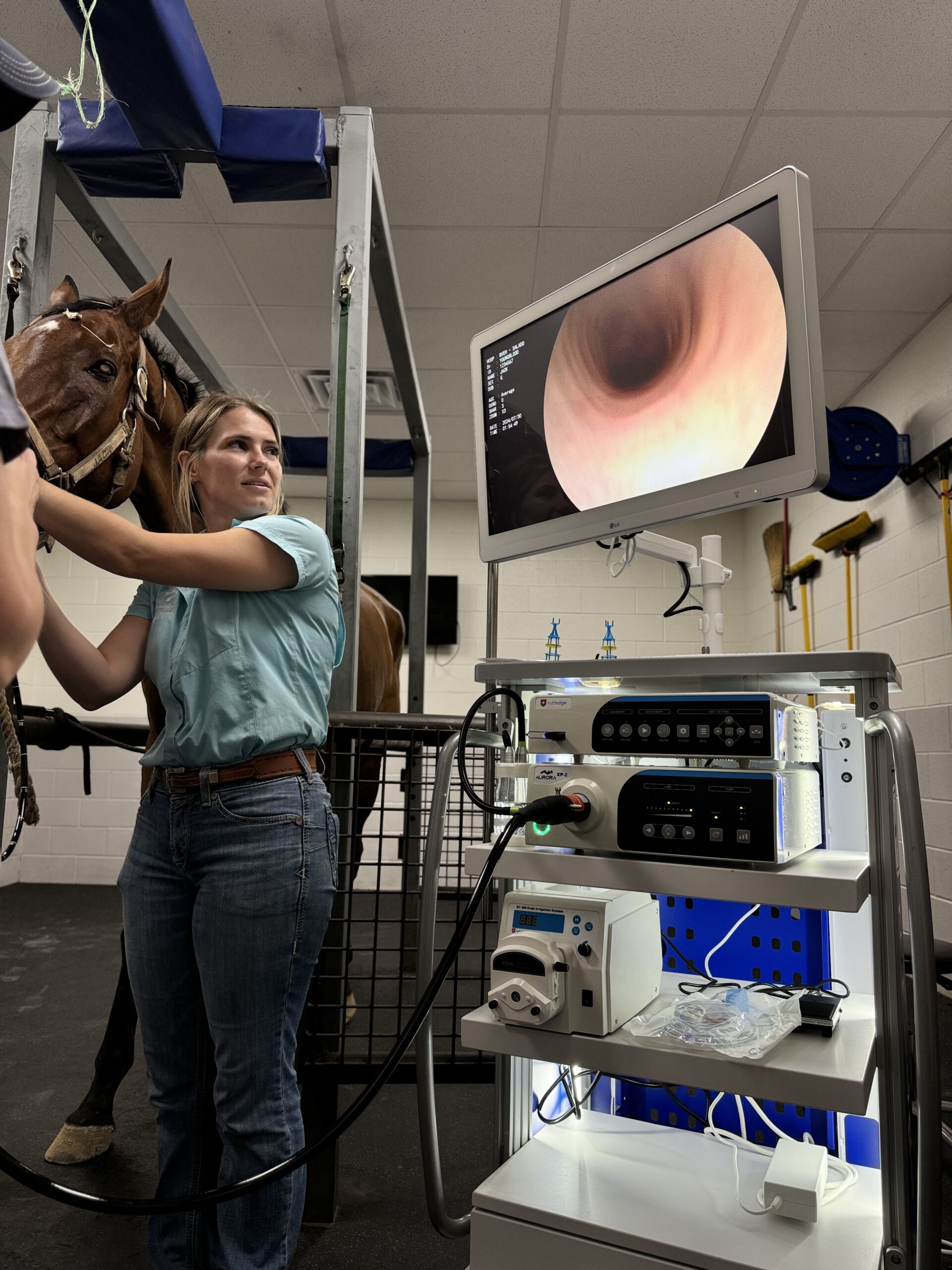
Infectious respiratory disease in horses carries both individual and herd-level risk. Whether it’s influenza, equine herpesvirus (EHV), Streptococcus equi (strangles), or other pathogens, delayed or imprecise diagnosis can cost time, health, and biosecurity. The AAEP’s 2025 Field Diagnostic Guidelines affirm that, in the workup of respiratory disease of unknown origin, endoscopy of the upper and lower airways is a key modality alongside imaging, swabs, nasal washes, and lavage techniques.

1. Why endoscopy is uniquely valuable
- Direct visualization of mucosal injury, lesions, and secretions. Many infectious agents produce characteristic signs—ulceration, edema, abnormal mucus, or purulent discharge—that may not be obvious on radiographs or ultrasound. Endoscopy reveals the airway’s actual condition in real time.
- Targeted sampling. Endoscopic guidance allows precise sampling (nasopharyngeal wash, tracheal wash, bronchoalveolar lavage, guttural pouch lavage) under visual control, minimizing contamination or blind sampling error.
- Assessment of upper airway involvement. Some agents affect the guttural pouches, dorsal pharynx, or laryngeal regions. Endoscopy allows access to these anatomic zones.
- Functional evaluation. Observing dynamic features like ciliary health, airway collapse, secretory flow, or subtle mucosal responses helps delineate infectious vs. inflammatory or allergic components.
- Biosecurity and outbreak mapping. Because infectious respiratory disease often requires isolation, knowing precisely which animal has airway lesions—and the severity—helps refine quarantine protocols and reduce unnecessary culling of asymptomatic horses.
Given these advantages, endoscopy is not merely optional in sophisticated practice settings; it is recommended in the AAEP’s diagnostic ladder, supplementing—but not replacing—other tests.

2. When endoscopy should come into play
In the AAEP flow chart for acute respiratory disease of unknown etiology, endoscopy is often triggered when:
- Multiple horses present with fever and respiratory signs, indicating potential infectious spread.
- You’ve ruled out simple, noninfectious causes (smoke exposure, allergies, EIPH) and need more granularity.
- Initial imaging or nasal swabs have been inconclusive, but the disease is progressive or high-risk.
- You must distinguish between infectious, inflammatory, and structural causes during outbreak management.
Because endoscopy is relatively low-risk (when sedation and safety protocols are followed), it serves as a natural next step when the initial clinical and laboratory workup doesn’t deliver a definitive answer.
3. Practical considerations and cautions
- Equipment and operator skill. Good endoscopic diagnosis demands excellent optics, flexible scopes, water/air channels, image capture, and a skilled operator familiar with respiratory anatomy and pathology. High Definition Video Endoscopes are Readily Available from several manufacturers.
- Infection control. Endoscope reprocessing is critical. With infectious disease, endoscopes and accessories must follow strict protocols to prevent spread. The use of High-level disinfectants or liquid sterilants approved for use with endoscopes is required. Enzymatic detergent is nOT a disinfection Chemical.
- Sampling hierarchy. Endoscopy should not replace standard swabs, washes, or clinical pathology—it complements them. The AAEP guidelines list it among diagnostic modalities, not the sole test.
- Cost-benefit balance. In some field settings with limited resources, endoscopy may be prohibitive; practices must weigh the incremental diagnostic yield vs. expense.
4. A model workflow for integrating endoscopy
- History & physical exam. Determine signs like fever, cough, discharge, travel, vaccination history.
- Initial diagnostics. Nasal swabs, PCR panels, CBC/chemistry, imaging (radiographs, thoracic ultrasound).
- Endoscopic evaluation. Inspect upper airway, guttural pouches, pharynx, trachea, bronchi.
- Targeted lavage and sampling. Collect sample under direct vision in areas of concern.
- Lab diagnostics. Send PCR, culture, cytology, fungal testing as needed.
- Management + biosecurity. Based on results, implement treatment, isolation, monitoring, and herd health measures.
5. Why pushing endoscopy matters
Veterinary practices that adopt endoscopy as a primary respiratory diagnostic tool gain several advantages:
- Faster diagnostic certainty. Analysts and clinicians don’t guess in the dark; they see pathology.
- Better therapeutic targeting. If you can distinguish viral vs. bacterial vs. fungal vs. structural causes early, you avoid overuse of broad-spectrum antibiotics, minimize treatment side effects, and preserve more lung health.
- Enhanced reputation and trust. Clients and referral centers value clinics that employ advanced diagnostics.
- Herd-level control. Identifying shedding animals or those with early lesions allows more precise quarantine, reducing outbreaks.
Conclusion
The AAEP’s 2025 guidelines rightly elevate endoscopy as part of the modern armamentarium for equine respiratory disease. When combined with imaging, cytology, and molecular diagnostics, it helps close the diagnostic gap that too often leaves horses treated empirically or with delays. For forward-thinking veterinary hospitals, making endoscopy a frontline tool in respiratory disease workups isn’t just recommended—it’s becoming expected.
READ THE GUIDELINES HERE: Equine Infectious Respiratory Disease Field Diagnostic Guidelines
